Radiofrequency ablation of atrial fibrillation by pulmonary vein isolation (PVI)
We use this patient information to welcome you to the Heart Clinic at Private Hospital Molholm and to provide you with information on radiofrequency ablation of atrial fibrillation.
Our staff will do their utmost to ensure that you feel safe and comfortable during your stay. Our aim is to combine professional treatment with good personal contact.
Between 85 and 90% of patients with episodic atrial fibrillation are helped by the treatment. If the atrial fibrillation is chronic or long-lasting, the anticipated success of the treatment is slightly less - around 70 %.
RFA (Radiofrequency ablation)
The purpose of this treatment is primarily to treat abnormal heart rhythm – named “atrial fibrillation”.
General information
What to bring
Toiletries, slippers and comfortable clothes. Also, bring your usual medication.
You do not strictly need being accompanied as you are permitted to carry a weekend bag with a change of clothes and toiletries and are also permitted to use public transport on your day of discharge – including travelling by airplane.
Medication
Continue taking your usual medication until your time of admission. This also applies if you take Marevan or Pradaxa/Eliquis/Xarelto/Lixiana.
The responsible cardiologist may also have assessed that there is no need for you to take blood-thinning medication prior to the ablation. However, you must always take this type of medication for a minimum of three months from your treatment.
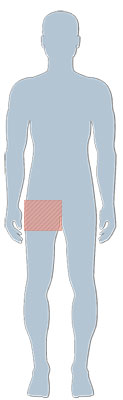
Shaving
Please shave your right-hand groin area using a single-use razor on the day prior to your admission as illustrated below:
Preparations at home (fasting)
You are not allowed to eat solid food for at least six hours prior to your appointment. You are permitted to drink until two hours prior to your appointment (avoid any dairy products).
You are not permitted to smoke less than two hours prior to your appointment.
Visiting hours and telephone contact
During your admission, your relatives may call the secretariat on telephone number +45 7642 7420.
Your spouse may be present at the hospital before, during and after treatment.
Mobile telephones are permitted.
On your day of admission
Preparing for your treatment
On your day of admission, you will be received by a nurse who will help you settle in and provide you with information about your hospital stay. You will be given the actual time of your surgery and specific precautions in connection with the surgery.
A line will be inserted into a vein in your arm. Your blood pressure and pulse will be measured, and blood samples may also be taken and an ECG may be performed.
Immediately prior to surgery, the responsible cardiologist will meat with you and inform you of any details, including any specific circumstances relating to your arrhythmia, which may impact the effect as well as any side effect of the surgery.
There will be plenty of time for this consultation and, naturally, your relatives are welcome to participate.
The procedure
The treatment takes approximately 2-3 hours. You will see a fair amount of technical equipment in the treatment room, such as computer screens and X-ray equipment.
Learn more about the use of X-rays here: X-rays (In Danish)
Prior to the catheter treatment being performed, a special ultrasound examination will be performed of your heart via your oesophagus (TEE). This is carried out to rule out any blood clots to be present at the inside of the left atrium despite the medicinal treatment with blood-thinning medicine. If clots have formed, there is a risk that these may detach during surgery which means that the surgery must be postponed. This examination is carried out during a brief general anaesthetic.
The remainder of the treatment is performed in a combination of local anaesthetics and heavy sedation. Catheters are threaded to your heart from the veins in your groin area. Using the catheters, the electrical impulses in your heart may be monitored. By increasing the temperature of the catheter tip to approximately 65⁰C, the cause of your arrhythmia is treated.
If you display atrial fibrillation during the surgery, we will endeavour to achieve normal cardiac rhythm (sinus rhythm) during the treatment by also applying an electric shock (DC conversion) to your chest.
Aftercare
After the procedure, all plastic tubes are removed and you will be monitored by a nurse for the next two hours, during which time you will need to lie flat on your back due to the risk of bleeding from the incision in your groin.
If you feel any discomfort, pain, sensations of heat or swelling in your groin area, you must tell the nurse of this.
Prior to discharge, your cardiologist will meat with you. This will be an opportunity to discuss any future precautions.
Discharge
Your incision will be checked.
You will receive the discharge papers and we will send a discharge letter with a description of the treatment to your general medical practitioner and the hospital which referred you for treatment.
Home transport
You are permitted to drive or to use public transport the day after the treatment. This includes air transportation.
Complications
In rare instances (a total risk of less than 1%), complications may arise: A significant accumulation of blood in your groin area incision, an accumulation of blood in your pericardium, air in your pleura, small blood clots in your vessels, in your heart or in other organs (brain, kidneys, lungs).
These complications may require observation or specialist treatment, which may be carried out locally.
When at home
The first week you must protect your groin by e.g. avoiding heavy lifting and long walks. Physical activities can therefore only be resumed one week after the treatment. However, we recommend to wait for another week before starting running, mountain bike/racing bike activities or golf playing.
You may return to work approximately one week after discharge. However, if your job is physically demanding, you must allow yourself two weeks’ recovery before going back to work.
Many patients have some pain/pressure/murmuring in the chest or light headaches the first few days after treatment, which can be managed with paracetamol 1 gram up to a maximum of 4 times daily - i.e. every 6 hours. Some may even experience migraine like reactions during the first couples of days. This is totally benign and nothing to worry about.
Aftercare
You may expect to develop a small bruise in the right-hand groin area around your incision. A few patients develop a slightly larger bruise (haematoma) which may be bothersome for a couple of weeks after the procedure.
Many patients have some pain/pressure/murmuring in the chest or light headaches the first few days after treatment, which can be managed with paracetamol 1 gram up to a maximum of 4 times daily - i.e. every 6 hours. Some may even experience migraine like reactions during the first couples of days. This is totally benign and nothing to worry about.
Usually, we recommend that you continue to take the heart-stabilising medication taken up to the procedure for an additional three months.
Similarly, you should continue to take your blood-thinning medication for at least three months after the procedure.
Changes to your medication should only be undertaken on the advice of your general medical practitioner or your cardiologist. It is particularly important that you consult your general medical practitioner before you stop taking you blood-thinning medication.
Some patients experience palpitations or atrial fibrillation after the procedure. This may be caused by an irritation of the cardiac scar tissue caused by the procedure and is not necessarily an indication of the procedure being ineffective. Some experience an increase in the number of attacks during the first 2-3 months after treatment, after which time the symptoms usually decrease. For this reason, the actual effectiveness of the procedure can only be ascertained after approximately three months or more.
It may be necessary to repeat the procedure. Experience states that approximately 15-20 % of patients require a further treatment to achieve the optimum result.
If you experience palpitations/atrial fibrillation, we suggest the following:
- If the symptoms are the same as before the procedure, wait and see if the attack spontaneously abates.
- If the symptoms are different than usual, you are recommended to seek assistance from your general practitioner with a view to having an ECG.
- If the attack is intolerable or lasts for more than 24 hours, you should be admitted to your local hospital with a view to having your cardiac rhythm regulated with medicine or with “electrical shock” treatment (DC conversion).
- In case of frequent relapses after surgery, a period of taking stronger heart medicine may be required to stabilise your cardiac rhythm. Your general practitioner may refer you to your local hospital with a view to changing your medication. In this situation, we often suggest prescription of Cordarone/Amiodarone for a 3-month period. This is well-tolerated by most patients without significant side effects.
It is a good idea to record the frequency and duration of any symptoms and bring this information to your outpatient check-up approximately three months after treatment.
Please seek immediate medical assistance in case of strong chest pains, difficulty breathing or fainting.
You are always welcome to call Privathospital Mølholm: +45 8720 3040
Specialists and practitioners